You may think that your late-night trips to the sweet cupboard are simply a matter of lacking willpower. However, research suggests that a microscopic mechanism may be at play, influencing your cravings in subtle yet powerful ways.
Emerging research suggests that your urges for evening sweets are biological, originating in your intestines and sent to your brain. This guide explores the link between gut health, microbiome restoration, and managing sugar cravings, equipping you to reclaim your diet and health.
To truly understand why you crave what you crave, it is important to move beyond calorie counting and investigate the complex ecosystem living within you. This next section explains why addressing gut health is crucial—not just for weight loss, but also for ending the ongoing chemical warfare in your digestive tract.
The Gut-Brain Axis: Who Is Really in Control?
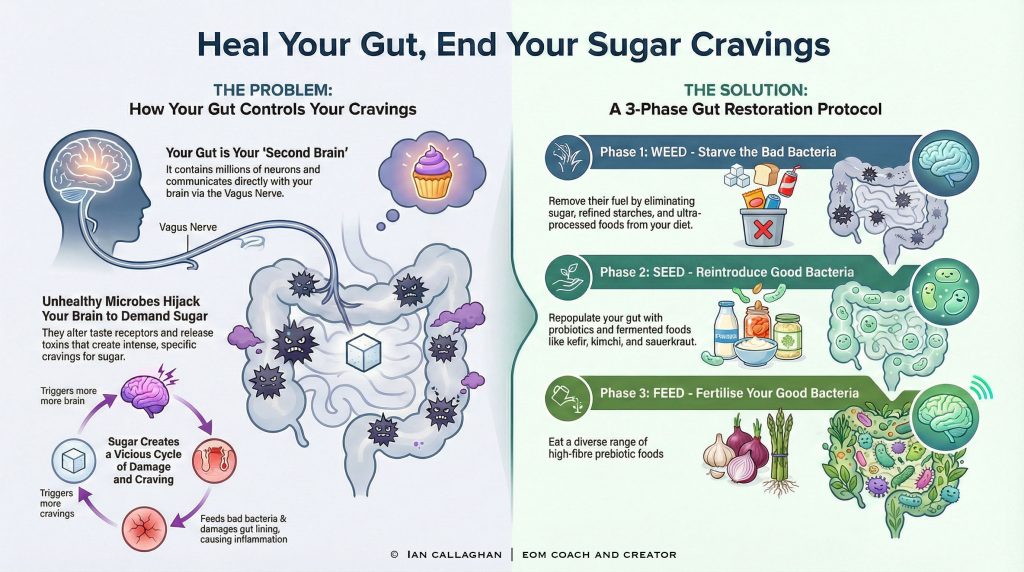
For decades, medicine treated the digestive system as a simple processing plant: food goes in, nutrients are extracted, and waste comes out. We now realise this view was dangerously simplistic. The gut is often referred to as the “Second Brain” because of the Enteric Nervous System (ENS), a mesh-like network of millions of neurons (nerve cells) lining your gastrointestinal (GI) tract (the pathway from your mouth to your anus).
This system communicates directly with your brain via the Vagus Nerve. Think of this nerve as a super-fast fibre-optic cable directly connecting your gut to your brain’s emotional and cognitive centres. While the brain sends signals to the gut (like the “butterflies” you feel when nervous), significantly more signals travel from the gut to the brain. The Vagus Nerve is one of the main nerves that control unconscious body processes, such as heart rate and digestion.
The Role of Neurotransmitters
The connection goes deeper than simple electrical signals. Your gut microbiome is a primary factory for neurotransmitters—the chemical messengers that dictate your mood, sleep, and appetite.
- Serotonin: Approximately 90% of your body’s serotonin—the “happy hormone”—is produced in the gut, not the brain.
- Dopamine: A significant portion of dopamine is also synthesised in the digestive tract.
- GABA: This calming neurotransmitter (a chemical that helps carry signals in the brain) relies heavily on beneficial gut bacteria for production.
When discussing microbiome restoration and managing sugar cravings, we’re referring to modulating key chemicals. An unbalanced microbiome leads to reduced serotonin levels, triggering sugar cravings for a quick boost.
Therefore, that sudden need for a biscuit or a sugary tea isn’t “greed”—it is your brain interpreting a chemical shortage caused by a dysfunctional gut environment.
Dysbiosis: The Root of the Sugar Trap
A healthy gut acts like a lush, diverse rainforest. It contains trillions of bacteria, fungi, and viruses that coexist in a delicate balance—a state known as eubiosis, where the gut microbes remain balanced and healthy. However, modern life—characterised by processed foods, antibiotics, chronic stress, and environmental toxins—can disrupt this balance, leading to a state called dysbiosis, where unhealthy microbes take over.
Dysbiosis occurs when pathogenic (bad) bacteria and yeasts crowd out the beneficial (good) bacteria. This is where the battle for your diet begins.
The Survival Instinct of Pathogens
Different microbes prefer different types of food. Beneficial bacteria, such as Bifidobacteria and Lactobacillus, thrive on dietary fibre found in vegetables, legumes, and whole grains. In contrast, pathogenic (disease-causing) bacteria and yeasts like Candida albicans thrive on simple sugars and refined starches.
This is the crux of the issue: microbes can manipulate host eating behaviour to increase their own fitness. This is known as the Microbiome Manipulation Hypothesis, which is the idea that gut microbes can influence human food choices to suit themselves. Pathogenic bacteria can:
- Alter Taste Receptors: They can change how you perceive taste, making high-sugar foods more palatable and healthy foods taste bland.
- Hijack the Vagus Nerve: They release toxins that travel up the Vagus nerve to stimulate the brain, creating intense cravings that only sugar can satisfy.
- Induce Dysphoria: When you attempt to quit sugar, these bacteria release toxins that make you feel anxious, jittery, or low—symptoms that vanish the moment you consume sugar and “feed” them.
Addressing gut health and sugar cravings is a strategic effort—not just habit-breaking, but eliminating an invasive population demanding sugar.
The Candida Connection
One of the most common culprits in severe sugar addiction is Candida albicans. While harmless in small amounts, this yeast can grow aggressively in a high-sugar, low-fibre environment. Candida is notorious for causing intense cravings for sweets, bread, and alcohol. It ferments these sugars to produce energy, creating a vicious cycle: the more sugar you eat, the more Candida grows, and the stronger the cravings become.
After learning about Candida, the next step is to identify whether microbiome restoration is needed in your own life.
Before embarking on a protocol, it is essential to recognise if your gut is indeed the source of your health struggles. Dysbiosis does not always manifest as stomach pain; often, the symptoms are systemic, affecting everything from your skin to your mental state.
If you resonate with three or more of the following indicators, your microbiome likely requires urgent attention.
1. Digestive Distress
This is the most obvious sign, yet many people ignore it, assuming bloating is “normal” after a meal. It is not.
- Chronic Bloating: Looking six months pregnant by the end of the day.
- Irregularity: Alternating between constipation and loose stools.
- Gas: Excessive or painful wind, particularly after eating carbohydrates.
- Reflux: Heartburn or indigestion that does not resolve with standard antacids.
2. Unexplained Fatigue and Brain Fog
When your gut is inflamed, your body expends a lot of energy mounting an immune response. Furthermore, pathogenic bacteria produce metabolic waste products (neurotoxins) that cross the blood-brain barrier.
- The Post-Lunch Slump: Needing a nap or caffeine immediately after eating.
- Mental Clarity Issues: Difficulty concentrating, poor memory, or feeling like you are thinking through treacle.
- Waking Up Tired: Feeling unrefreshed even after a full night’s sleep.
3. Skin Conditions
The skin is often a mirror of the gut. This is referred to as the Gut-Skin Axis. When the gut cannot eliminate toxins effectively, the body attempts to push them out through the skin.
- Adult Acne: Particularly cystic acne around the jawline.
- Eczema and Rosacea: Chronic gut inflammation manifests as skin inflammation.
- Psoriasis: Strongly linked to intestinal permeability (Leaky Gut), a condition where the gut lining becomes too porous, allowing unwanted substances to enter the bloodstream.
4. Immune System Fragility
Approximately 70% of your immune system resides in your gut. If your microbiome is compromised, your defences are down.
- Frequent Colds: Catching every bug that goes around the office.
- Autoimmune Issues: Conditions such as Hashimoto’s or Rheumatoid Arthritis are often exacerbated by gut dysbiosis.
5. The Sugar Reliance
As discussed, this is the key behavioural indicator.
- Inability to Stop: Once you start eating sweets, you cannot stop until the packet is empty.
- Mood Swings: Becoming “hangry” or anxious if you miss a meal or haven’t had sugar recently.
The Sugar-Gut Feedback Loop: A Vicious Cycle
Successfully managing microbiome restoration and sugar cravings requires understanding the mechanical harm sugar causes to the gut. Sugar not only feeds harmful bacteria but also degrades the gut barrier.
Intestinal Permeability (Leaky Gut)
The lining of your intestine is only one cell thick. These cells are held together by “tight junctions.” In a healthy gut, these tight junctions act like a security guard, allowing nutrients to pass into the bloodstream while keeping out toxins, undigested food particles, and pathogens (harmful microbes).
High sugar consumption promotes inflammation that loosens these tight junctions. This condition is known as Intestinal Permeability, or Leaky Gut.
When the gut becomes “leaky,” the following cascade occurs:
- Lipopolysaccharides (LPS) Leakage: LPS are toxins found in the cell walls of bad bacteria. When they leak into the bloodstream, they cause systemic (whole body) inflammation.
- Immune Response: Your immune system marks these unwanted particles as foreign invaders and attacks them. This constant state of alert leads to chronic (long-lasting) fatigue and autoimmunity (when the body attacks its own tissues).
- Blood-Brain Barrier Breach: The systemic inflammation can eventually weaken the blood-brain barrier, leading to neuroinflammation—manifesting as anxiety, depression, and intensified cravings.
The Insulin Rollercoaster
When you consume high-sugar foods to satisfy a craving driven by dysbiosis, your blood glucose spikes. Your pancreas releases insulin to shuttle this sugar into cells. However, because the spike is so high, the subsequent drop is severe. This crash (hypoglycaemia) triggers a panic signal in the brain: “We need fuel now.”
The result? Another intense craving for sugar.
This creates a dual-layered trap:
- Biological: The bad bacteria demand sugar for their survival.
- Metabolic: Your unstable blood sugar demands energy to prevent a crash.
Breaking this cycle requires a multi-faceted approach. You cannot simply use “willpower” to fight physiology. You must repair the machinery.
The Impact of Modern “Food” on the Microbiome
It is important to define what we are fighting against. The modern Western diet (often called the Standard American Diet, though the UK is not far behind) is catastrophic for gut health. It is not just sugar; it is the entire chemical cocktail found in ultra-processed foods.
Emulsifiers and Artificial Sweeteners
You might think switching to “sugar-free” diet drinks is the answer to managing sugar cravings. Unfortunately, this often backfires.
- Artificial Sweeteners: Substances like aspartame, sucralose, and saccharin have been shown to be bacteriostatic—they can inhibit the growth of beneficial gut flora. Furthermore, because they taste sweet but provide no calories, they confuse the brain’s reward centre, often leading to increased cravings for real sugar later.
- Emulsifiers: Common additives like polysorbate-80 and carboxymethylcellulose (found in ice cream, spreads, and sauces) act like detergents in the gut. They strip away the protective mucus layer that shields your gut lining, accelerating Leaky Gut and inflammation.
The Fibre Deficit
The average UK adult consumes roughly 18g of fibre per day, well below the recommended 30g. Fibre is the primary fuel source for your beneficial bacteria (prebiotics). Without adequate fibre, your good bacteria starve.
When beneficial bacteria starve, they cannot produce Short-Chain Fatty Acids (SCFAs), specifically Butyrate. Butyrate is a miracle molecule that:
- Repairs the gut lining (tight junctions).
- Lowers inflammation.
- Regulates metabolism.
- Signals satiety (fullness) to the brain.
Low fibre intake + high sugar intake = a perfect storm for dysbiosis. The good guys starve, and the bad guys feast.
Preparing for Restoration: The “Weeding” Phase
Before we can plant a new garden (reintroduce good bacteria), we must clear the weeds (reduce pathogenic overgrowth). In the context of Gut Health & Nutrition: Microbiome restoration and managing sugar cravings, this is often the most challenging phase because the “weeds” will fight back.
This phase is not about starvation; it is about strategic elimination. The goal is to remove the primary inflammatory triggers and the fuel sources for pathogenic bacteria.
The Die-Off Reaction (Herxheimer Reaction)
As you begin to starve pathogenic bacteria and yeast by removing sugar, they die. As they die, they release endotoxins into your system. This can lead to a temporary worsening of symptoms known as a “die-off” reaction.
- Symptoms: Headaches, flu-like symptoms, fatigue, and irritability.
- Duration: Typically 3 to 7 days.
- Management: Hydration and sweating (exercise/sauna) are crucial during this time to help the body eliminate toxins.
Understanding that this reaction is a sign of success, not failure, is vital for persistence. When you feel terrible three days after quitting sugar, it is physical proof that the pathogenic bacteria are dying.
End of Part 1. The following sections will cover the “Seeding” and “Feeding” phases, detailed dietary protocols, supplement strategies, and lifestyle changes required to permanently restore the microbiome and banish sugar cravings.
SEO TITLE
Restoring Gut Health: How To Stop Sugar Cravings?
HOOK
Clearing the weeds is futile if you fail to replant the garden, making the seeding and feeding phases of Gut Health & Nutrition: Microbiome restoration and managing sugar cravings the most critical factors for long-term success.
Phase 2: The “Seeding” Phase (Reinoculation)
Once the pathogenic overgrowth has been dampened by the “weeding” phase, the gut environment is akin to a ploughed field. It is clear, but it is vulnerable. If we do not introduce beneficial species immediately, the resilient weeds (sugar-loving bacteria) will simply return, often more aggressively than before.
In the context of Gut Health & Nutrition: Microbiome restoration and managing sugar cravings, the seeding phase introduces diversity. A monoculture in the gut is a sign of ill health; a diverse ecosystem is a sign of resilience.
Probiotics: The Reinforcements
Probiotics are live bacteria and yeasts that are good for you, especially your digestive system. However, not all probiotics are created equal. To combat sugar cravings, we need strains that influence satiety hormones and mood regulation.
- Lactobacillus & Bifidobacterium: These are the most researched genera. Specifically, Lactobacillus rhamnosus has been shown to assist in weight management and reducing cravings associated with anxiety.
- Saccharomyces boulardii: This is actually a beneficial yeast. It acts as a place-holder, occupying space on the gut wall to prevent pathogenic yeast (like Candida) from re-attaching while your native bacteria recover.
- Spore-Based Probiotics: Unlike traditional probiotics found in yoghurt, spore-based (soil-based) organisms are encased in a natural shell that allows them to survive stomach acid and reach the colon intact. They are particularly effective for “re-terraforming” the gut.
Fermented Foods: The Ancient Method
While supplements provide high doses of specific strains, fermented foods provide a complex matrix of bacteria, enzymes, and organic acids.
- Sauerkraut and Kimchi: Rich in Lactobacillus. Ensure these are unpasteurised and refrigerated; shelf-stable versions are usually dead.
- Kefir: A fermented milk drink that is far more potent than standard yoghurt. Coconut water kefir, or water kefir, is an excellent alternative for those avoiding dairy.
- Miso and Tempeh: Fermented soy products that support the microbiome.
Action Step: Introduce fermented foods slowly. Start with one teaspoon of sauerkraut juice per day. Jumping straight into a bowlful can cause significant bloating and discomfort if your gut isn’t accustomed to it.
Phase 3: The “Feeding” Phase (Prebiotics)
You have weeded the garden and planted the seeds. Now, you must fertilise the soil. Probiotics are the seeds; prebiotics are the fertiliser. Prebiotics are types of dietary fibre that the human body cannot digest. They travel to your lower digestive tract, where they act as food for the healthy bacteria.
This is a critical juncture in Gut Health & Nutrition: Microbiome restoration and managing sugar cravings. If you take probiotics but continue to eat a low-fibre diet high in processed foods, the new bacteria will starve and die, and the cravings will return.
The Role of Short-Chain Fatty Acids (SCFAs)
When your good bacteria ferment prebiotic fibre, they produce Short-Chain Fatty Acids (SCFAs), specifically butyrate, acetate, and propionate.
- Butyrate: The primary fuel source for the cells lining the colon. It reduces inflammation and strengthens the gut barrier (healing “Leaky Gut”).
- Appetite Regulation: SCFAs travel to the brain and signal satiety. High levels of SCFAs are directly linked to reduced sugar cravings because the body feels chemically satisfied.
Top Prebiotic Foods to Include
To optimise for Gut Health & Nutrition: Microbiome restoration and managing sugar cravings, incorporate the following “fertiliser” foods:
- Chicory Root: Roughly 47% inulin fibre.
- Dandelion Greens: Excellent for liver support and gut flora.
- Jerusalem Artichokes: High inulin content (start slow).
- Garlic, Onions, and Leeks: The Allium family is potent fuel for beneficial flora.
- Asparagus: A great source of prebiotic fibre.
- Green Bananas: Unripe bananas are high in resistant starch, which behaves like soluble fibre.
Dietary Protocols for Restoration
Moving beyond simple lists of foods, we must look at the overall dietary strategy. The modern British diet often relies heavily on beige carbohydrates—such as toast, pasta, and sandwiches—which break down immediately into glucose. To restore the microbiome, we must shift the macronutrient balance.
The “Crowding Out” Principle
Trying to “stop eating sugar” is a psychological battle based on deprivation. “Crowding out” is based on abundance. By filling your plate with nutrient-dense proteins, healthy fats, and high-fibre vegetables, there is physically no room left for sugar, and metabolically, the body ceases to crave it.
The Importance of Healthy Fats
Fat is essential for microbiome restoration. Unlike sugar, fat does not spike insulin significantly. It provides a slow-burning fuel source that keeps energy levels stable, preventing the crash-and-burn cycle that triggers sugar cravings.
- Include: Avocados, extra virgin olive oil, coconut oil, nuts, seeds, and oily fish (mackerel, salmon, sardines).
- Avoid: Highly processed seed oils (sunflower, soybean, rapeseed), which can be pro-inflammatory.
The Power of Bitter Foods
In modern cuisine, we have largely eliminated the bitter taste profile, favouring sweet and salty. However, bitter receptors in the gut play a role in the release of satiety hormones (CCK and GLP-1).
- Protocol: Eat something bitter before a meal to prime digestion and curb sweet cravings.
- Foods: Rocket, radicchio, endive, grapefruit, or a splash of apple cider vinegar in water.
Supplement Strategies for Gut Repair
While food is the foundation, specific supplements can accelerate repair of the intestinal lining (mucosa) and help manage withdrawal symptoms from sugar cessation.
L-Glutamine
L-Glutamine is the most abundant amino acid in the body and is the preferred fuel source for the cells of the small intestine. Supplementing with L-Glutamine helps to “seal the leaks” in the gut lining, reducing systemic inflammation.
- Dosage: typically 2–5 grams per day, dissolved in water.
Magnesium Glycinate
Sugar consumption depletes magnesium. Paradoxically, magnesium deficiency increases sugar cravings, creating a vicious cycle.
- Benefit: Magnesium Glycinate is highly absorbable and gentle on the stomach. It helps regulate blood sugar levels and manages the anxiety/irritability associated with the “weeding” phase.
Zinc Carnosine
Zinc is crucial for immune function and gut integrity. The carnosine form is specifically researched for its ability to adhere to the stomach and gut lining, promoting repair and preventing permeability.
Lifestyle Factors: The Gut-Brain Axis
We cannot discuss Gut Health & Nutrition: Microbiome restoration and managing sugar cravings without addressing the lifestyle factors that influence the microbiome. The gut and the brain are connected via the Vagus nerve. Stress in the brain causes chaos in the gut, and chaos in the gut sends anxiety signals to the brain.
Stress Management
When you are stressed, your body releases cortisol. High cortisol levels increase gut permeability (“Leaky Gut”) and alter the composition of gut bacteria, often killing off the good guys and encouraging the growth of pathogens.
- The Vagus Nerve: Activities that stimulate the Vagus nerve can switch the body from “fight or flight” to “rest and digest.”
- Techniques: Deep diaphragmatic breathing, humming, cold water exposure (finishing your shower with 30 seconds of cold water), and meditation.
Sleep and the Circadian Rhythm
Your microbiome has a circadian rhythm. The bacteria function differently day and night. Poor sleep or erratic eating windows (late-night snacking) disrupt this rhythm.
- Protocol: Aim for 7–9 hours of sleep. Try to finish eating at least 3 hours before bed to allow the gut to perform its “housekeeping” waves (Migrating Motor Complex), which sweep bacteria out of the small intestine.
Movement and Diversity
Studies suggest that athletes have a more diverse microbiome than sedentary individuals. Exercise increases the production of butyrate (the beneficial fatty acid). You do not need to run a marathon; a daily brisk walk or resistance training is sufficient to boost microbial diversity.
Long-Term Maintenance: Preventing Relapse
Restoring gut health is not a 30-day programme; it is a lifestyle shift. Relapse occurs when old habits creep back in—the daily biscuit with tea, the processed sandwich for lunch.
To maintain a healthy microbiome:
- The 80/20 Rule: If you eat whole, microbiome-supporting foods 80% of the time, your gut flora will likely be resilient enough to handle the occasional treat without triggering a full-blown craving relapse.
- Rotate Foods: Do not eat the same five vegetables every week. Aim for 30 different plant foods per week (herbs, spices, nuts, seeds, veg, and fruit all count). Diversity on the plate equals diversity in the gut.
- Listen to Your Body: If bloating returns, or if you feel a sudden spike in sugar cravings, treat it as a warning light on the dashboard. Revert to the “Weeding” phase for a few days to reset.
Conclusion
The connection between Gut Health & Nutrition: Microbiome restoration and managing sugar cravings is undeniable. Sugar cravings are rarely just a lack of willpower; they are often a biological signal from a distressed microbiome. By following the Weeding, Seeding, and Feeding protocol, you are not just dieting; you are engaged in ecosystem management.
You are restoring the internal balance of power. When the beneficial bacteria thrive, they reward you with stable energy, mental clarity, and a natural indifference to the sugary treats that once controlled you. The journey to restoring your health begins in the gut, and the result is a life where you, not your microbes, are in control of your dietary choices.